- 0 Comments
- Health
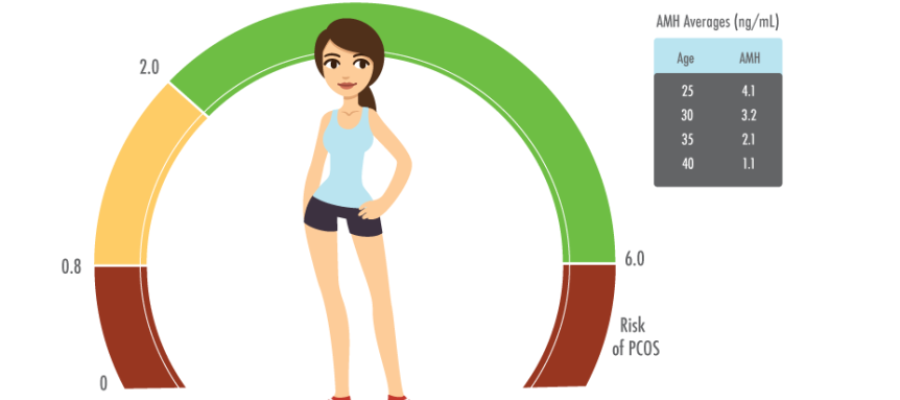
MYTHS AND FACTS ABOUT INFERTILITY Female age does not matter as long as you are under 35 years of age? FALSEWomen are born with a limited number of eggs that declines with age. This results in a measurable decline in fertility that begins in mid-20’s and becomes progressively steeper after 30’s. After 40’s the chance of successful live birth with a woman’s own egg is extremely low.However, the rate of depletion of eggs may be rapid in some women as compared to their counterparts in the same age group. I am maintaining a healthy lifestyle with respect to regular exercise, healthy food and mindful activities so nothing can affect my fertility. It’s a mythA healthy body and mind do help boost your fertility, but cannot reverse the effects of aging on your ovaries and your sperms. Other pathological factors causing infertility like infections (tuberculosis, PID), azoospermia, varicocele, blocked fallopian tubes or uterine malformations cannot be prevented with a healthy lifestyle alone. We have sex daily so our chances of getting pregnant are higher. FalseHaving sex everyday does not increase the chances of pregnancy compared to those having intercourse every alternate day or during the fertile window. Being on birth control pills for longer periods leads to infertility. It’s a mythOral contraceptive pills are usually safe and do not cause infertility. Couples can plan pregnancy 2-3 months after stopping the pill. However, intra-uterine devices like copper-T may sometimes induce infection or cause swelling in the uterus, leading to infertility. If you have conceived once and had a healthy pregnancy in the past you cannot be infertile. It’s a mythIssues such as uterine changes post-delivery, infections, or a decline in ovarian reserve may cause secondary infertility. Semen parameters may also be affected over time due to various factors. Males do not have a biological clock. MythAlthough men can produce sperm throughout life, sperm quality declines with age. Increased male age is associated with reduced semen quality and increased risk of miscarriage due to greater DNA fragmentation. Infertility is only a woman’s problem. FalseMale and female infertility are equally prevalent. 35% of infertility cases are due to male factors, 35% female, 10% combined, and 20% unexplained. Putting your legs up after intercourse or avoiding standing up after sex will improve your chances of conception. MythGravity does not affect sperm movement. They reach the fallopian tube on their own. Infertility is mostly the problem of the West and affects only a small population in India. FalseOne in 10 couples in India faces infertility. Lifestyle changes, late marriages, obesity, smoking, drinking, and drug use increase risk. Coffee has no impact on fertility; I need to stop caffeine only once I am pregnant. False Women consuming more than 2 cups of coffee daily have reduced fertility. Caffeine is present in coffee, tea, colas, and chocolates. All women have 28-day cycles and ovulate on day 14. FalseOnly 16% of women have a 28-day cycle. Ovulation typically occurs 14 days before the next period. It’s advisable to have intercourse every alternate day from day 8 to cover the fertile window. Obesity has no effect on fertility. FalseObesity causes hormonal imbalances that affect ovulation in women and sperm production in men. Some sexual positions increase your chances of getting pregnant. ProbablyThere is no conclusive evidence, but deep penetration positions like missionary may deposit sperm closer to the cervix. Laptops can impair sperm production. TrueHeat from laptops used on the lap can reduce sperm production and quality. An average couple conceives within 3 months of trying. False85% of couples conceive within a year. Those who don’t should seek fertility evaluation. Stress does not affect fertility or conception. FalseChronic stress impacts hormone levels and sperm production, causing issues with ovulation and implantation. Women ovulate during every menstrual cycle. FalseAnovulatory cycles (no egg release) are common, especially in women with endometriosis or PCOS. Every fertility journey looks the same. FalseFertility depends on age, time trying to conceive, ovarian reserve, tubal patency, and semen parameters. Each couple’s journey is unique.